Just a friendly heads-up! The information shared in this post is for general knowledge purposes only and should not be considered a substitute for professional medical advice. It’s crucial to talk to a healthcare professional before trying any new supplements. They can provide personalized guidance based on your unique needs and ensure they are safe for you. Remember, your health comes first, so consult with a qualified healthcare provider for the best advice tailored to you.
Table of Contents
This article may contain compensated links. Please read Disclaimer for more info. As an Amazon Associate, I earn from qualifying purchases.

In the dead of night, you’re playing a lonesome game of stare-down with the clock. Minutes morph into a battlefield of endless hours.
This nightly duel sounds familiar? Then welcome to the ever-swelling ranks of the sleepless.
Insomnia isn’t your one-off restless night; it’s a relentless marathon of wakefulness. The stats are startling. 10% of people deal with this chronically, while up to 35% experience occasional bouts.
This is where Cognitive Behavioral Therapy for Insomnia (CBT-I) steps in. It could be the lifeline you need, guiding you back to restful sleep.
Did you know that you can access science-backed CBT-I online from the comfort of your home?
In this article, we will look at some cunning, evidence-based online tools that can help you create better nights and brighter days.
Jump directly to the best online CBT-I program recommendations.
What is Cognitive Behavioral Therapy for Insomnia (CBT-I)
Before we get to the recommendations for online CBT-I tools, let us quickly define: What is CBT?
Other than sleep disorders, cognitive behavioral therapy (CBT) is a successful treatment for a variety of conditions. It has been shown to be highly effective in treating conditions like personality disorders, eating disorders, substance abuse, PTSD, and anxiety disorders.
CBT-I is all about tackling the stress and emotional issues that often come with insomnia. Plenty of research proves it’s a healthier and more effective choice compared to sleep aids like supplements or prescription meds.
So, what’s behavioral sleep medicine all about?
CBT-I has one clear goal: to help you build healthier sleep habits.
It’s meant to help you identify and change the root patterns and behaviors that contribute to your insomnia. Therapy is based on the notion that your brain is capable of learning new, advantageous responses to stimuli.
High success rates make it an attractive option, particularly for those whose insomnia may be intertwined with mental health issues like anxiety.
During CBT-I sessions, you’ll delve into your thoughts and behaviors around sleep. But the therapy doesn’t end with the sessions. You’ll be guided to keep a sleep diary and practice strategies by yourself to solidify new habits.
(Check out the free sleep diary downloadable below.)

Components of CBT-I
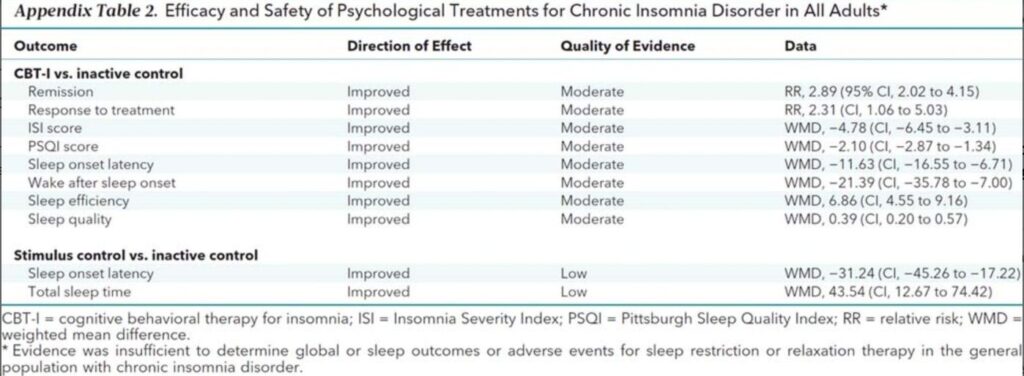
The American Academy of Sleep Medicine and the American College of Physicians both recommend clinical management of insomnia using cognitive therapy as the go-to treatment.
Here’s what it involves:
- Sleep Restriction: Establish and strictly adhere to a sleep routine, with fixed sleep and wake times. Initially, you might feel under-rested with CBT-I sleep restriction, but the idea is to train your brain to associate bed with sleep.
- Stimulus Control: Understand and manage environmental factors affecting sleep, like noise, light, and temperature. Strive for a dark, quiet, and cool sleeping environment and limit bed use to sleep and intimacy.
- Relaxation Training: This is especially helpful for those prone to stress and anxiety. Techniques such as progressive muscle relaxation, deep breathing exercises, meditation, and visualization can promote physical and mental relaxation before sleep.
- Paradoxical Intention: This technique asks you to intentionally stay awake while following good sleep hygiene rules. It can be particularly useful for those struggling with sleep anxiety.
- Biofeedback: Used with or without a biofeedback device, this method helps you become aware of and manage physiological responses like heart rate or muscle tension, which may be influenced by sleep-related anxieties.
- Cognitive Restructuring: This technique works by identifying and replacing irrational or negative thoughts about sleep. By shifting to more rational and positive thought patterns, you can change how you relate to sleep.
- Sleep Hygiene: Consistent, good sleep hygiene is key. This means a regular sleep schedule, a conducive sleep environment, and avoidance of stimuli like caffeine and electronics near bedtime.
A comprehensive review in 2015, encompassing over 20 different CBT-I trials, revealed that insomniacs who used these CBT-I techniques fell asleep 20 minutes quicker on average and spent 30 fewer minutes awake overall compared to those who didn’t.
However, remember that therapy is not a one-size-fits-all solution. The effectiveness of each technique can vary and it might take some time and patience to see improvements.
Why Use CBT-I Instead of Medication?
Several types of medications may provide temporary relief from insomnia. Over-the-counter sleep med and prescription sedatives are common, but these should be considered short-term solutions.
Despite their potential to offer respite during intense insomnia episodes, these medications have potential drawbacks like the “hangover” effect, tolerance build-up, dependency, and a range of side effects from headaches and dizziness to nausea.
Even antidepressants, while sometimes helpful in sleep regulation, can take months to show results and may paradoxically impair sleep quality.
Therefore, CBT-I shines as a preferable alternative to medication.

The Digital Revolution in Insomnia Treatment: Benefits of CBT Insomnia Online
If you’re grappling with persistent sleep issues, you’ve likely realized that “Dr. Google” doesn’t provide the comprehensive solution you need. What’s required is a structured, systematic approach.
However, with the number of qualified CBT-I providers estimated to be no more than 200, there’s a clear shortage when considering the 60 million Americans suffering from insomnia. And the global shortage is even worse.
Online cognitive behavioral therapy for insomnia has emerged as a potential solution. As an online service, it can scale and meet overwhelming demand.
While traditional therapy offers a neutral space and non-verbal cues, it can be pricey and less accessible. Online therapy, on the other hand, is convenient and accessible, but relies on good internet and may not suit severe conditions.
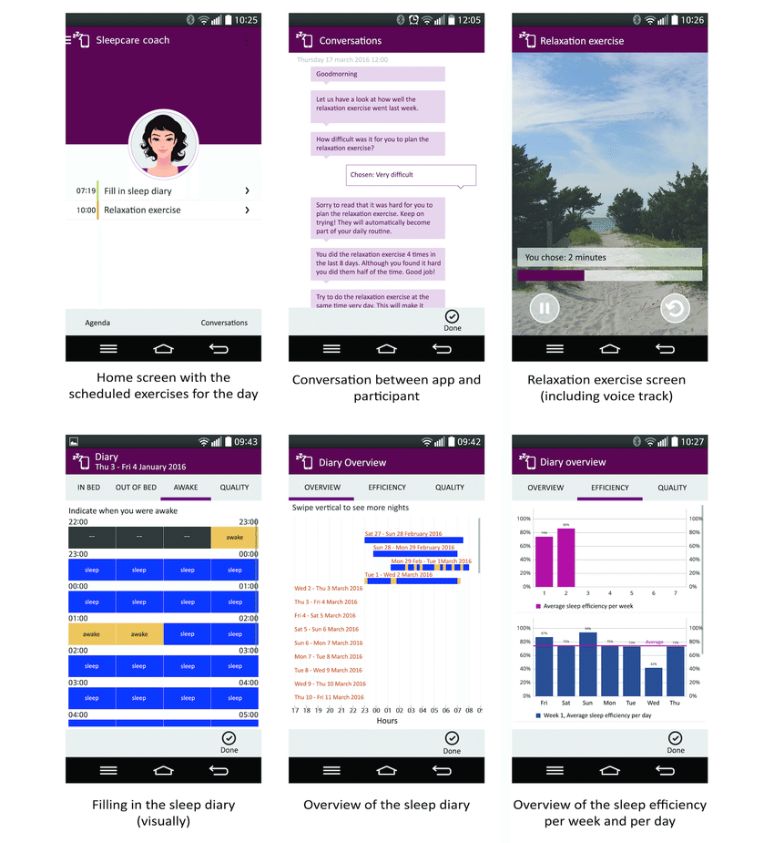
In 2017, scientists put a Dutch automated mobile app delivering CBT for insomnia under the microscope. Almost 150 sleep-challenged individuals took part. The result? Those who used CBT-I training online saw a major boost in sleep quality.
The best part? These improvements were still going strong three months down the line.
So, the American Academy of Sleep Medicine made the decision to support and recommend
online CBT insomnia programs as a treatment due to extensive scientific evidence.
A 2016 review of 15 trials showed sleep improvements with insomnia CBT online programs across the board: a 7.2% boost in sleep efficiency, less severe insomnia, an extra 20 minutes of sleep, and even a decrease in depression symptoms.
Another 2016 meta-analysis of 14 studies gave it the same thumbs up.
The verdict on all these studies? CBT-I online is not just on par with traditional programs; it’s a game-changer.

Advantages and Disadvantages of Online CBT-I and In-Person CBT-I
To get you started navigating the world of therapy, let’s weigh the pros and cons of online CBT-I and in-person CBT-I. Here’s a quick rundown to help you make an informed choice.
In-person CBT-I:
Pros:
- Accountability: Regular meetings with a therapist provide motivation and commitment.
- Accurate Diagnosis: Trained therapists can identify symptoms of underlying conditions causing insomnia.
- Sustainability: Lower dropout rates are associated with in-person therapy, promoting long-term success.
- Non-Verbal Cues: Therapists can interpret body language and non-verbal signals, enhancing the therapy process.
- Human Interaction: Personal contact can enhance the comfort and effectiveness of therapy.
Cons:
- Availability: Locating a qualified therapist can be difficult.
- Scheduling: Therapy sessions must align with both the patient’s and therapist’s schedules.
- Commute: Traveling to therapy sessions can be time-consuming and stressful.
- Flexibility: Rescheduling missed sessions can be challenging.
- Cost: In-person therapy can be expensive, depending on insurance coverage.
Online CBT-I:
Pros:
- Global Access: Your CBT-I course is available anywhere with an internet connection.
- Convenience: Therapy can be conducted from the comfort of home.
- 24/7 Availability: Online CBT-I is accessible at any time, accommodating all sleep schedules.
- Cost-Effective: Depending on insurance, online therapy may be more affordable than traditional methods.
- Privacy: Online therapy offers a high degree of anonymity and confidentiality.
Cons:
- Self-Motivation Required: Progress is largely self-directed without a physical therapist to report to.
- Higher Dropout Rate: Participants may be more likely to discontinue online programs prematurely.
- Limited Scope: Online CBT-I may not be sufficient for insomnia caused by underlying conditions.
- Technical Difficulties: Unstable internet connections can interrupt therapy sessions.
- Less Personal: Online programs may lack the personal touch of in-person therapy.
While online CBT-I has many advantages, it might not be the best fit for everyone. Consider these situations:
- Serious Mental Health Conditions: If you’re dealing with conditions like severe depression, bipolar disorder, or schizophrenia, it’s important to consult your doctor before starting online CBT-I.
- Sleep Disorders: If your insomnia is due to conditions like sleep apnea or restless legs syndrome (RLS), these need to be addressed first.
- Certain Medical Conditions: Dealing with chronic pain or certain neurological conditions might require a more comprehensive treatment approach.
- Cognitive Impairment: If you have significant cognitive impairment or dementia, online CBT-I might be less effective.
- Motivation: Online CBT-I requires active participation. If you’re not ready for change, it might not be the right choice for you.
When in doubt, it’s always best to talk to your healthcare provider.

Unveiling the Top Digital CBT-I Solutions
Let’s dive into the world of online CBT-I solutions, a field where technology and healthcare unite to combat insomnia.
It’s important to note that not all products in this market are created equal. They generally fall into three categories: Approved Digital Therapeutics (DTx), scientifically validated solutions, and user-endorsed options.
We will highlight seven outstanding performers from the first two categories in this overview. These substitutes have received scientific backing and have undergone clinical testing. They use empirical tools such as the Insomnia Severity Index (ISI) to assess the intensity of your sleep issues and track your progress throughout the course.
Please note that we have no affiliations with any of these digital CBT-I programs, ensuring our reviews are completely unbiased.
Here they are:
- Somryst™
- Sleepio
- CBT-i Coach
- Restore
- A Mindful Way to Healthy Sleep
- This Way Up
- CBTforInsomnia.Com
Somryst™, previously known as SHUTi, is a digital therapeutic tool crafted to assist those grappling with insomnia. It stands out as the only solution that has earned clearance from the U.S. Food and Drug Administration (FDA).
While it does come with a high price tag, some health insurance providers do cover these costs.
Backed by robust clinical support, Somryst™ requires a prescription and is designed to be used under the guidance of a healthcare professional. It’s specifically targeted at managing “chronic insomnia.”
Having undergone a revamp and rebranding, this innovative program now offers an even more engaging and effective way to tackle insomnia.
Somryst’s Approach:
Think of Somryst™ as your personal sleep trainer. The app offers a comprehensive program that spans up to nine weeks. It includes six core lessons designed to help you fall asleep faster and stay asleep longer.
The program focuses on constant feedback and personalization. It tracks your progress and shares this information with your healthcare provider, ensuring your records are always up-to-date.
The program has a sound design and has shown to be both secure and efficient. However, it does have some demanding parts. Particularly during the second week, you’ll be asked to restrict your sleep window.
But remember, persistence is key. With time, you’ll reap the benefits of better sleep.
Pricing:
For a nine-week supply of Somryst™, you’re looking at a price tag of 899 USD.
But here’s some good news—your insurance might cover it. If it doesn’t, eligible patients have the option to use a Somryst Savings Card to bring the cost down to as low as 100 USD. You can pay in one go or split it into three equal payments.
If you have a Flexible Spending Account (FSA) or Health Spending Account (HSA), you can use those funds too.
Scientific Evidence:
Somryst™ has a proven track record of improving sleep, as evidenced by the National Institute of Health studies.
In 2018, Pear Therapeutics acquired SHUTi and in March 2020, obtained FDA market authorization for the digital therapeutic for insomnia.
Multiple studies show that users who complete the program sleep 6.4 more hours per week and spend 43% less time falling asleep and 55% less time awake at night.
Another recent study revealed that the Somryst™ program can help reduce symptoms of depression, suicidal ideation, and anxiety in individuals at risk of depression.
Who is Somryst™ for?
Somryst™ is designed for individuals aged 22 or older suffering from chronic insomnia. You should also be under the supervision of a healthcare provider in the United States.
Somryst™ uses sleep restriction and consolidation, which may worsen certain preexisting medical conditions. If you have any conditions or disorders that could be aggravated by sleep restriction you should not use Somryst™. These include parasomnias, epilepsy, untreated obstructive sleep apnea, bipolar disorder, schizophrenia, and untreated obstructive sleep apnea.

Launched in 2012, Sleepio is based on 30 years of clinical and research experience by Colin Espie, PhD.
Although it has a wealth of clinical evidence supporting it and is acknowledged as a Digital Therapeutics (DTx) product, it still lacks an FDA label.
You can only get Sleepio through your employer, and it’s designed for you to use on your own. So, there’s no need for a doctor to get involved, except in certain situations where there might be contraindications.
Sleepio’s Approach:
After a short onboarding sleep questionnaire, Sleepio provides a tailored program with an animated cartoon therapist known as “The Prof.”
Over the course of six weeks, you’ll log in weekly for a 20-minute session with The Prof. In between sessions, you can practice CBT for insomnia techniques and complete your sleep diary.
Sleepio also includes access to educational materials and an online user community. There are additional features like relaxation MP3s, sleep progress reports, email reminders, and more.
Pricing:
Sleepio costs 400 USD for an entire year. But if you agree to participate in a research study or it is already covered by your employer’s health insurance, you might be able to get it for free.
The program offers a 100% money-back guarantee.
Scientific Evidence:
Reliable clinical data is used to support Sleepio. As the gold standard in clinical research, it has been tested in a randomized controlled trial with a placebo group. The results of this trial were published in the highly respected peer-reviewed journal SLEEP in June 2012.
The findings were impressive. Sleepio has been shown to help those struggling with sleep in several ways.
It can help users fall asleep up to 50% faster and reduce nighttime awakenings by up to 60%. Not only that, but it can also boost daytime energy and concentration levels by up to 50% and help users achieve a more consistent sleep pattern.
The Lancet, one of the world’s leading medical journals, published a commentary on the clinical trial. They hailed Sleepio as “a proven intervention for sleep disorders using the internet…from www to zzz.”
Further studies are available in full text on the official Sleepio website.
Who is Sleepio for?
Sleepio is a program designed for those who regularly face difficulties falling asleep, maintaining sleep, or waking up too early.
However, it’s not a quick fix. It requires a commitment over several weeks and a readiness to put in some effort.
It’s important to note that Sleepio isn’t suitable for everyone. If you’re dealing with unstable mental or physical health, it might not be the right choice. It’s not recommended for pregnant women, children, shift workers, or those who feel excessively sleepy during the day.
And remember, Sleepio isn’t a replacement for professional medical advice. If you’re uncertain about starting the program, or if you have a pre-existing medical condition or are on medication, it’s wise to consult your doctor first.
The good news is that Sleepio isn’t limited to the USA and UK. It’s accessible in several other countries as well. So, if you’re struggling with sleep, Sleepio could be just a few clicks away, no matter where you are.
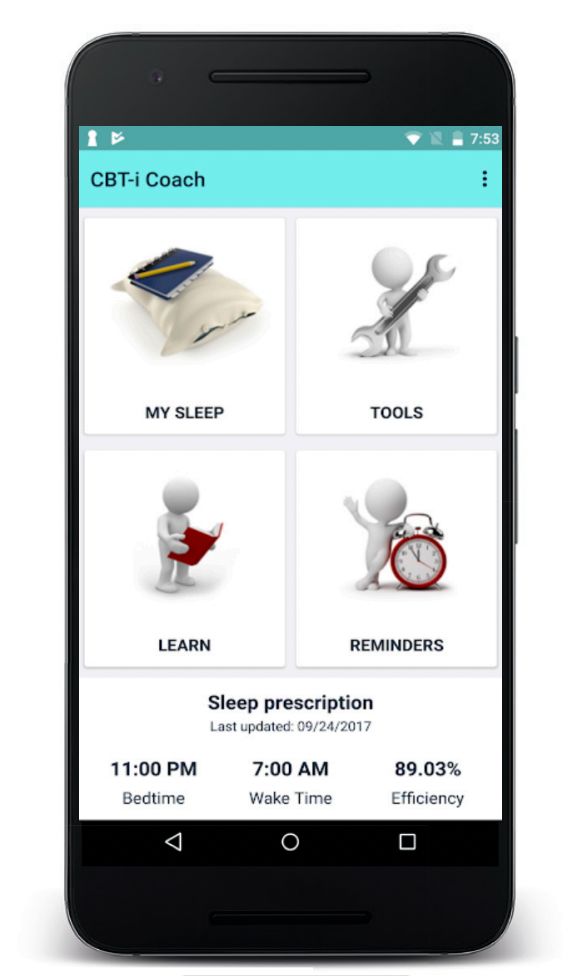
CBT-i Coach is a free mobile app designed as a digital supplement to help patients in face-to-face CBT-I. It was launched in 2013 by the National Center for PTSD of the US Department of Veterans Affairs as a tool to help soldiers manage chronic insomnia disorder from PTSD.
The National Center for Telehealth and Technology of the DoD and the Stanford School of Medicine collaborated to create the app. As of 2014, the app had claimed 30,000 users.
CBT-i Coach’s Approach:
The CBT-I app offers a structured program to help reset your biological clock, making it easier for you to fall asleep and stay asleep throughout the night.
It’s packed with features like sleep education, tips for developing positive sleep routines and improving sleep environments, a sleep diary to track your sleep times, and tools to help you relax when you’re getting ready for sleep or trying to go back to sleep.
The goal of CBT-i Coach is to supplement in-person care from a medical professional. While it can be used independently, it’s not intended to replace therapy for those who need it.
If you’re not currently seeing a provider for CBT-I, there’s also the Insomnia Coach, another free app that guides you through good sleep habits.
Pricing
This CBT insomnia app is completely free and available for iOS and Android phones—both for veterans and civilians.
Scientific Evidence
The coach is based on the official CBT-I manual, Cognitive Behavioral Therapy for Insomnia in Veterans.
The U.S. Department of Veterans Affairs found in a study that CBT-I clinicians trained by the VA have a favorable opinion of the app. In fact, 60% of them use it with their patients to increase commitment to tasks and boost performance.
Who is CBT-i Coach for?
This CBT-I sleep app is designed for people who are engaged in Cognitive Behavioral Therapy for Insomnia with a health provider or who would like to improve their sleep habits.
The primary users are a subset of chronic insomnia patients, namely US veterans with PTSD who are directed to the product by the VA.
However, the app is technically accessible to anyone and only requires an app download. It’s worth noting that the Coach is commonly found in the top results of Google with the terms “insomnia app”.

Restore is another readily available online sleep aid that will help you get a good night’s rest. Launched in 2006 by Cobalt Therapeutics, it’s a bilingual (English and Spanish) CBT-I solution.
Developed under the expertise of Dr. Norah Vincent, Restore has been making waves in the sleep science community, with its effectiveness showcased in a randomized, controlled trial published in the Journal SLEEP.
Restore’s Approach:
Restore is a personalized, 7-session sleep program that can be finished in as little as 5 weeks.
It provides a wealth of informational resources. You can download CBT for insomnia handouts and sleep hygiene worksheets. There are videos and audio clips to help you learn about good sleep hygiene, stress management, and relaxation methods.
You’ll be encouraged to maintain a digital sleep diary and practice the techniques demonstrated in the program. Plus, you can download audio clips of a sleep therapist and an actor in a staged one-to-one session, allowing you to revisit the contents at your convenience.
Pricing:
Restore offers three pricing tiers to suit your needs and budget.
- The Silver tier (£99.00) includes printable CBT-I worksheets and reminder emails.
- The Gold tier (£229.00) adds a 60-minute coaching session and clinician support to the mix.
- And the Platinum tier (£179.00) is the all-inclusive package, offering additional resources to help manage panic and phobias, OCD, diet, and depression, along with the features of the Silver and Gold tiers.
Scientific Evidence:
There is a wealth of scientific evidence supporting the Restore program’s efficacy. Cobalt Therapeutics, the creators of Restore, reports that 80% of those who complete the program see significant improvements in their insomnia symptoms.
A study published in the journal Sleep in 2009 supports this claim. It found that 81% of adults with chronic insomnia experienced at least mild improvement after the 5-week Restore program. Over 30% were even sleeping a full hour more at the end of the program.
However, the dropout rate was 33%, slightly higher than traditional therapy.
But don’t let that deter you. Since then, 10 more studies led by Dr. Norah Vincent, PhD, have replicated these positive results. All these studies are available for download in full-text on the Restore website.
Who is Restore for?
Restore is made for adults who struggle with sleep issues. Restore could be a great fit for you if you prefer a self-guided, online approach to treating your insomnia. The online format allows you to work around your schedule, making it a convenient option if you find it challenging to attend in-person therapy sessions.

A Mindful Way to Healthy Sleep is another online sleep improvement program offering a drug-free approach to treating insomnia. Created by qualified Clinical Psychologists of Australia, it combines CBT-I with mindfulness training, all grounded in over 35 years of clinical research.
A Mindful Way’s Approach:
This cutting-edge online course, A Mindful Way to Healthy Sleep, focuses on the root causes of sleep problems. The program offers tips for improving overall wellness and sleep quality.
What sets this program apart is its unique blend of CBT-I and mindfulness. It’s the first of its kind to integrate these two approaches.
The course incorporates seven key principles of mindfulness, each contributing to healthier sleep patterns. These principles include acceptance, non-judging, trust, patience, non-striving, and letting go.
The course consists of six modules, delivered once a week for six weeks. You can sign up for the six-week course online, watch video lessons, complete daily practices, and practice new skills, including daily mindfulness practices.
You’ll learn all the tricks according to this CBT-I protocol:
- Identify and manage the underlying causes of insomnia.
- Modify activities and habits that disrupt sleep and develop new healthy sleep habits.
- Create a personalized sleep schedule.
- Quiet and calm the mind to prevent anxious thoughts during the night.
- Recognize and change unhelpful thinking patterns about sleep.
- Apply effective techniques for relaxing the body before sleep.
- Manage stress and fatigue during the day with practical techniques.
- Prevent chronic insomnia from reoccurring with tools to maintain healthy sleep habits.
Pricing:
A Mindful Way to Healthy Sleep is priced at 297 AUD.
This one-time payment grants you immediate access to the program and a full 12 months to explore and benefit from its resources. The package includes weekly video lessons and action points, downloadable meditation recordings, and lesson summaries in a CBT-I workbook.
If you wish, feedback about your progress can be sent to your doctor. Plus, if you’re not satisfied with the program, there’s a 7-day money-back guarantee, giving you the freedom to try it out risk-free.
Scientific Evidence:
In a first-of-its-kind randomized controlled trial, Monash University independently assessed A Mindful Way to Healthy Sleep.
The study found it to be significantly more effective at reducing insomnia than a waitlist control group. On the Insomnia Severity Index (ISI), 83% of people who completed the program achieved clinical improvement in insomnia, and 75% achieved full remission of insomnia.

The integration of mindfulness into this program is rooted in scientific evidence highlighting its benefits for sleep. For instance, one study found that after participating in a six-week mindfulness course, a whopping 87% of participants reported improved sleep.
This finding isn’t alone; numerous other studies have consistently shown that practicing mindfulness positively impacts sleep quality.
Who is A Mindful Way for?
This program is particularly beneficial for those who appreciate the mindfulness approach to tackling insomnia.
While A Mindful Way is designed to be helpful for most, it’s not recommended for individuals currently experiencing serious mental health issues, those under the age of 16, pregnant women, or new parents with an infant.
In order to combat insomnia, This Way Up teaches practical CBT-I techniques. It is especially useful if you have previously received an insomnia diagnosis but have not tried CBT.
This Way Up’s Approach
This Way Up’s is a comprehensive toolkit designed to help you tackle insomnia head-on.
While it’s primarily focused on improving sleep, the program integrates the principles of the management of mood and anxiety disorders.
Anxiety can lead to a restless mind, making it challenging to fall asleep or maintain sleep. Similarly, mood disorders like depression can disrupt sleep patterns. Therefore, it can be very helpful to incorporate CBT-I treatment methods into the treatment of these disorders.
The program uses techniques like cognitive restructuring and stress management, which are effective at managing these disorders. These strategies help address mental and emotional factors to improve sleep.
The course is divided into four story-based lessons. Each one teaches you a practical skill to help break the cycle of insomnia.
Here’s what you’ll be diving into:
- The Science of Sleep and Understanding Your Insomnia: Get to grips with the science behind sleep and gain a deeper understanding of your insomnia.
- Managing Sleep-Interfering Thoughts and Behaviors Part 1: Learn how to manage those pesky thoughts and behaviors that interfere with your sleep.
- Managing Sleep-Interfering Thoughts and Behaviors Part 2: Continue building on the strategies from the previous lesson to further improve your sleep.
- Reviewing Your Skills and Maintaining Your Gains: Review everything you’ve learned and discover how to maintain your progress.
- Alongside these lessons, you’ll have access to a range of extra resources and tools to help you overcome common challenges. You’ll also receive a CBT insomnia workbook filled with exercises designed to help you tackle your symptoms.
To keep you on track, you’ll get reminder emails and texts, and you’ll have insomnia patient handouts with step-by-step activities to help you put your new skills into practice.
Pricing:
The program is free for a limited time, after which it’ll cost you 59 AUD. However, if a clinician prescribes the program, it stays free. Plus, it’s available to people residing in Australia and worldwide with a prescription.
Scientific Evidence:
For more than ten years, This Way Up has created and distributed evidence-based online mental health programs. Numerous scientific studies support their effectiveness.
All of their programs are created by experienced clinical psychologists and are based on validated CBT manuals and clinical practice guidelines. Their treatment programs have been put to the test in clinical trials and have shown to significantly reduce symptoms and functional impairment.
Who is This Way Up for?
This Way Up’s program could be a good fit if you:
- Have been finding it increasingly difficult to fall or stay asleep over the last 3 months
- Experience broken or restless sleep, and find it hard to get up in the morning
- Want to learn cognitive therapy exercises for anxiety and depression to improve sleep
- Feel tired the next day even after getting enough hours of sleep
- Feel stuck in your current cycle and are ready and willing to learn new skills to change the way you feel.

CBTforInsomnia.com, also known as the Conquering Insomnia Program, was launched in 2005. This trailblazer in the realm of online CBT-I has been helping people conquer sleepless nights for over a decade.
The mastermind behind this program is Dr. Gregg D. Jacobs, a renowned CBT-I and sleep specialist. The program is based on his 20 years of research and clinical practice in sleep medicine at Harvard Medical School.
Conquering Insomnia is a product of Jacobs’ groundbreaking research, funded by the National Institutes of Health (NIH). His studies have shown that CBT-I programs can outperform even popular sleep aids like Ambien.
CBTforInsomnia.com’s Approach:
The Conquering Insomnia Program is a five-week course, with each week focusing on a different field of CBT-I. The course is designed to be self-guided and includes the following components:
- Understanding and changing beliefs about sleep
- Lifestyle habits that improve sleep
- Developing relaxation and stress reduction skills
- Changing sleep schedules
- Preventing insomnia in the future
The program is supplemented with additional resources such as workbooks, action plans, and progress tracking tools.
Pricing:
The Conquering Insomnia Program is available in three pricing tiers:
Basic (49.95 USD)
Plus (54.95 USD)
Premium (69.95 USD)
All contain downloadable PDFs. The Plus program also includes a 20-minute MP3 download of guided muscle relaxation, breathing, and visualization techniques. The Premium program includes the MP3 as well as five email Q&A sessions with Dr. Jacobs. Additional products incorporate a CBT insomnia manual and webinars for clinicians, as well as a standalone 60-minute MP3 program.
Scientific Evidence:
The programs are based on Dr. Jacobs’s widely-cited 2004 research at Harvard Medical School of the effectiveness of CBT-I. The 63 young and middle-aged adults with chronic sleep-onset insomnia who participated in the study reported:
- 85% improvement in sleep
- 80% reduction in reliance on sleeping pills
- 70% increase in total sleep time, up to a full hour
- Fewer nights of insomnia overall
However, it’s worth noting that there aren’t specific studies on the effectiveness of the online program. But, Dr. Jacobs does share CBT insomnia success stories and testimonials on his website and has reported a very low refund request rate.
Who is CBTforInsomnia.com for?
If you’re struggling with insomnia and are looking for a structured, evidence-based approach to improve your sleep, this could be a good fit. Furthermore, it’s also a great resource for clinicians seeking training materials on CBT-I.
However, keep in mind that some users have reported a lack of support and poor customer service, so it might not be the best choice for everyone.
The program gets its users from a combination of both physician referrals and self-referrals.

Conclusion
Navigating through the sea of online programs and apps for battling insomnia can be quite a journey. It’s tough to figure out which ones stick to the CBT-I playbook and are truly effective.
In this article, we’ve aimed to spotlight those digital therapeutics that have research on their side.
The range of options is vast—from the high-end, FDA-approved Somryst™ to the simple yet potent CBT-i Coach app, there’s something to fit everyone’s wallet.
Sure, the FDA-approved choices might not be many, but having solutions that are research-based and evidence-backed is already a big plus. And let’s not forget the less expensive or even free options.
But these digital tools aren’t magic wands. And they’re not one-size-fits-all solutions.
Keep in mind that some might need a prescription or a health care provider’s supervision. Others might not be suitable if you have certain medical conditions.
So, before you jump in, it’s worth having a chinwag with your healthcare provider or mental health professional.
Investing in a solution that works for you is like investing in a healthier, more fulfilling life.
So, why not give it a shot? A good night’s sleep is just a few clicks away.

Key Concepts and FAQ on Digital CBT-I
CBT is the acronym for what term?
CBT stands for Cognitive Behavioral Therapy, a type of psychotherapy that helps individuals understand how their thoughts (cognition) and actions (behavior) affect their feelings and overall well-being.
What is CBT used for, and what does CBT involve?
CBT can treat anxiety, depression, PTSD, insomnia, and other psychological disorders. To have CBT explained simply, it involves a practical, goal-oriented approach where patients learn to identify and change destructive thought patterns that have a negative influence on behavior and emotions, ultimately aiding in treating these mental health conditions.
Cognitive Behavioral Therapy. Does it work?
Absolutely. Cognitive behavioral education has been scientifically proven to be effective in managing various psychological disorders. CBT provides individuals with tools to identify, challenge, and change their unhealthy thought patterns and behaviors, which contributes to their recovery and resilience.
What is CBT training? What aspects does it include?
CBT in a nutshell: This approach teaches the principles and techniques of cognitive-behavioral therapy. It covers the CBT rules of identifying negative thought patterns, understanding their impact on emotions and behavior, and implementing changes.
What’s a typical example of a CBT therapy session?
A typical CBT therapy session may involve discussing the client’s current issues, identifying negative thought patterns, and learning new strategies to manage these thoughts. A CBT model example might include setting homework for the patient to apply these techniques in daily life.
When is CBT used for insomnia?
CBT is used for insomnia when the condition becomes chronic or recurrent. It’s based on the “insomnia theory” that certain cognitive and behavioral factors can perpetuate sleep problems. CBT-I aims to change these unhelpful thoughts and behaviors, improving sleep quality.
Is CBT-I for insomnia effective?
Yes, CBT-I is recognized as a highly effective treatment for chronic insomnia. Whether delivered in-person or through online CBT programs, it can significantly improve sleep quality, reduce the time it takes to fall asleep and decrease night-time awakenings when adhered to consistently.
When was CBT-I insomnia established? And who invented CBT-I?
CBT-I, or Cognitive Behavioral Therapy for Insomnia, was developed in the late 20th century, evolving from traditional Cognitive Behavioral Therapy. It’s been a collective effort of many psychologists and researchers over the years, with Arthur Spielman contributing significant work on the “3-P model” (Predisposing, Precipitating, and Perpetuating factors) that underpins CBT-I.
What are some examples of CBT techniques in relation to insomnia?
CBT techniques for insomnia include stimulus control therapy, sleep restriction, sleep hygiene, relaxation training, and cognitive therapy. Each is designed to address a specific aspect of insomnia, and together, they can significantly improve sleep quality.
Give an example of a CBT session for insomnia.
A typical example of a CBT session for insomnia begins with understanding the patient’s sleep habits through a detailed discussion or sleep diary analysis. The therapist will then educate the patient about healthy sleep and the role of behaviors, environment, and cognition in fostering it.
Together, they’ll work on techniques such as sleep restriction therapy, stimulus control, cognitive restructuring, and relaxation training. These are all aimed at reshaping detrimental beliefs about sleep, building a healthy sleep routine, and promoting relaxation.
Progress is then monitored, and strategies are adjusted accordingly in subsequent sessions.
What is CBT not good for if you’re suffering from insomnia? Can CBT be harmful?
While CBT is generally safe and effective for treating insomnia, it may not work for everyone. It requires active participation and engagement, which may be challenging for some. In some cases, focusing on negative thoughts and experiences can be distressing, but this is usually a temporary phase of therapy. It’s essential to understand the limitations of behavioral therapy for insomnia and CBT requirements before starting.
For instance, CBT-I might not be the best course of action for individuals with certain health conditions, such as bipolar disorder or schizophrenia. Moreover, it’s typically not recommended for pregnant individuals or those under the age of 16.
Are there risks to doing cognitive behavioral therapy for insomnia online?
Online Cognitive Behavioral Therapy for Insomnia, or CBT-I online, can have risks if not properly administered or followed. Misinterpretation or misapplication of CBT insomnia self-help techniques can occur. However, if implemented correctly, online CBT-I can provide valuable tools to help manage insomnia.
Can I access CBT for insomnia online free? Are there free CBT-I therapy apps?
Yes, some platforms offer online free CBT-I. For example, “CBT-i Coach” is an evidence-based, high-quality option. However, the effectiveness of some other free resources can vary, so it’s crucial to select a program from a reputable source.
Why access Cognitive Behavioral Therapy insomnia online?
Accessing CBT-I online provides convenience, flexibility, and often more affordability than traditional in-person therapy. Online platforms can offer a structured therapy program that can be accessed anytime, from anywhere, making therapy more accessible to those who may otherwise have limited resources or time. While online resources can be helpful, they are not a replacement for professional medical advice.
How do you find the best CBT locations for insomnia treatment if you want to get 1 to 1 therapy?
Finding the best CBT locations for insomnia treatment involves research and consultation. Look for accredited mental health clinics or hospitals offering CBT services, and consider factors like the therapist’s experience, specialization, and patient reviews.
However, in the digital age, an increasing number of insomniacs are helped by online therapy too, which broadens the choices available.
How long does it take for CBT-I to work?
The time it takes for CBT-I to show results varies based on individual circumstances. However, with consistent application of the key components of CBT and by implementing CBT tips and strategies, many people start noticing improvements within a few weeks to a few months.
How does the CBT triangle apply to insomnia?
The CBT triangle, representing thoughts, feelings, and behaviors, is used in treating insomnia by helping individuals identify and challenge their negative thoughts about sleep. The triangle helps to understand feelings of anxiety or frustration related to sleep and provides insights into how to modify behaviors that contribute to insomnia.
Are CBT interventions for anxiety and insomnia related?
The management and modification of negative thoughts and behaviors is a common theme in both CBT interventions for anxiety and insomnia. In many cases, anxiety can be the cause or consequence of insomnia. Therefore, CBT techniques for insomnia often include strategies to manage anxiety, which contributes to the “cognitive behavioral therapy for sleep anxiety”.
Are CBT interventions for depression and insomnia related?
Yes, depression and insomnia are often co-occurring conditions. CBT techniques used to treat depression, such as challenging negative thought patterns and promoting positive behaviors, can also be effective in managing insomnia.
What are the rules of golden sleep?
The rules of golden sleep or good sleep hygiene include maintaining a regular sleep schedule, creating a relaxing bedtime routine, and making your sleep environment comfortable. Furthermore, you should avoid large meals, caffeine, and alcohol before bedtime, and engage in regular physical activity.
CBT, DBT. What is better for insomnia?
Both CBT (Cognitive Behavioral Therapy) and DBT (Dialectical Behavioral Therapy) can be effective in treating insomnia. However, CBT-I is specifically designed for insomnia and is considered the gold standard of treatment. DBT may be helpful when insomnia is a symptom of another mental health condition, like borderline personality disorder.
What’s the CPT code for cognitive behavioral therapy for treating insomnia?
The Current Procedural Terminology (CPT) code for cognitive behavioral therapy for insomnia will depend on the specifics of the service provided. It’s best to consult with a medical billing professional or your healthcare provider to determine the correct CPT code for insomnia treatment. For general cases, the CPT code for cognitive behavioral therapy for insomnia is 90808.
As a psychologist, where do I get CBT-I training?
A number of accredited institutions and organizations offer CBT-I certifications for psychologists. You may also become a CBT instructor through these programs. Some prestigious options include the Oxford Cognitive Therapy Centre and other similar institutions that offer CBT insomnia training. However, exercise caution because not all programs will prepare you to practice as a cognitive behavioral therapist for treating insomnia.
How much do behavioral therapists make if they have a CBT-I specialization?
The salary of behavioral therapists with a CBT-I specialization varies based on factors like location, years of experience, and the complexity of the cases they handle. Generally, therapists with specialized skills like CBT-I can command higher salaries due to their specialized knowledge and the demand for these services.
What do digital therapeutics clinical trials show about insomnia treatment?
Digital therapeutics (DTx) clinical trials show promising results for insomnia treatment. Many digital therapeutics companies have developed apps that offer CBT-I and have demonstrated efficacy comparable to face-to-face therapy in clinical trials. This supports the growing adoption of digital therapeutics platforms for insomnia treatment.
What are the requirements for digital therapeutics software?
Requirements for digital therapeutics software include scientific validation, user-friendly design, data security, and regulatory compliance. With a focus on digital therapeutics mental health, these platforms need to provide accurate and effective interventions, while also ensuring the privacy and safety of users.
What are some digital therapeutics examples?
Examples of digital therapeutics include applications that deliver cognitive-behavioral therapy for various conditions like insomnia, depression, and anxiety. They provide interventions often equivalent to face-to-face therapy and illustrate the benefits of digital therapeutics such as increased accessibility, affordability, and convenience.
What’s the CBT Institute? Is there a center for cognitive behavioral psychotherapy?
The CBT Institute refers to various organizations around the world that offer cognitive-behavioral therapy services and training. Similarly, there are centers for cognitive behavioral psychotherapy that provide therapy services, training, and research opportunities. One example is the “Centre for Clinical Interventions,” which provides resources and training on various psychological disorders, including sleep hygiene for insomnia.

Sources
Cognitive Behavioral Therapy for Chronic Insomnia: A Systematic Review and Meta-analysis: Annals of Internal Medicine: Vol 163, No 3. Annals of Internal Medicine. Published 2015. Accessed July 30, 2023. https://www.acpjournals.org/doi/10.7326/M14-2841.
Horsch C, Jaap Lancee, Fiemke Griffioen-Both, et al. Mobile Phone-Delivered Cognitive Behavioral Therapy for Insomnia: A Randomized Waitlist Controlled Trial. 2017;19(4):e70-e70. doi:https://doi.org/10.2196/jmir.6524.
Clinical Management of Insomnia Using Cognitive Therapy. Behavioral Sleep Medicine. Published 2023. Accessed August 5, 2023. https://www.tandfonline.com/doi/abs/10.1207/s15402010bsm0403_4.
Online Cognitive Behavioral Therapy is Effective in Treating Chronic Insomnia – American Academy of Sleep Medicine – Association for Sleep Clinicians and Researchers. American Academy of Sleep Medicine – Association for Sleep Clinicians and Researchers. Published June 2009. Accessed July 30, 2023. https://aasm.org/online-cognitive-behavioral-therapy-is-effective-in-treating-chronic-insomnia/.
Seyffert M, Pooja Lagisetty, Landgraf J, et al. Internet-Delivered Cognitive Behavioral Therapy to Treat Insomnia: A Systematic Review and Meta-Analysis. 2016;11(2):e0149139-e0149139. doi:https://doi.org/10.1371/journal.pone.0149139.
Ye Y, Chen N, Chen J, et al. Internet-based cognitive–behavioural therapy for insomnia (ICBT-i): a meta-analysis of randomised controlled trials. 2016;6(11):e010707-e010707. doi:https://doi.org/10.1136/bmjopen-2015-010707.
Morin CM. Profile of Somryst Prescription Digital Therapeutic for Chronic Insomnia: Overview of Safety and Efficacy. Expert Rev Med Devices. 2020 Dec;17(12):1239-1248. doi: 10.1080/17434440.2020.1852929. Epub 2020 Dec 2. PMID: 33226269.
Elison S, Ward J, Williams C, et al. Feasibility of a UK community-based, eTherapy mental health service in Greater Manchester: repeated-measures and between-groups study of “Living Life to the Full Interactive”, “Sleepio” and “Breaking Free Online” at “Self Help Services.” 2017;7(7):e016392-e016392. doi:https://doi.org/10.1136/bmjopen-2017-016392.
Espie, C.A., Kyle, S.D, Williams, C., Ong, J.C., Douglas, N.J., Hames, P., Brown, J.S.L. (2012). A randomized, placebo-controlled, trial of online Cognitive Behavioral Therapy for chronic Insomnia Disorder delivered via an automated media-rich web application. SLEEP 35, 769-781.
Espie CA, Carl JR, Stott R, Henry AL, Miller CB. Digital medicine needs to work. Published online December 1, 2018. doi:https://doi.org/10.1016/s0140-6736(18)32519-4.
Kuhn E, Weiss BJ, Taylor KL, Hoffman JE, Ramsey KM, Manber R, Gehrman P, Crowley JJ, Ruzek JI, Trockel M. CBT-I Coach: A Description and Clinician Perceptions of a Mobile App for Cognitive Behavioral Therapy for Insomnia. J Clin Sleep Med. 2016 Apr 15;12(4):597-606. doi: 10.5664/jcsm.5700. PMID: 26888586; PMCID: PMC4795288.
Vincent N, Lewycky S. Logging on for better sleep: RCT of the effectiveness of online treatment for insomnia. Sleep. 2009 Jun;32(6):807-15. doi: 10.1093/sleep/32.6.807. PMID: 19544758; PMCID: PMC2690569.
A Randomized Controlled Trial to Examine the Feasibility and Preliminary Efficacy of a Digital Mindfulness-Based Therapy for Improving Insomnia Symptoms. Springer.com. Published 2023. Accessed August 1, 2023.
Jacobs GD, Pace-Schott EF, Stickgold R, Otto MW. Cognitive behavior therapy and pharmacotherapy for insomnia: a randomized controlled trial and direct comparison. Arch Intern Med. 2004 Sep 27;164(17):1888-96. doi: 10.1001/archinte.164.17.1888. PMID: 15451764.
Behavioral and psychological treatments for chronic insomnia disorder in adults: an American Academy of Sleep Medicine clinical practice guideline | Journal of Clinical Sleep Medicine. Journal of Clinical Sleep Medicine. Published 2021. Accessed August 4, 2023. https://jcsm.aasm.org/doi/10.5664/jcsm.8986.
Management of Chronic Insomnia Disorder in Adults: A Clinical Practice Guideline From the American College of Physicians | Annals of Internal Medicine. Annals of Internal Medicine. Published 2016. Accessed August 4, 2023. https://www.acpjournals.org/doi/10.7326/M15-2175.
Prescription sleeping pills: What’s right for you? Mayo Clinic. Published 2022. Accessed August 4, 2023. https://www.mayoclinic.org/diseases-conditions/insomnia/in-depth/sleeping-pills/art-20043959.
CLARK MS, SMITH PO, JAMIESON B. Antidepressants for the Treatment of Insomnia in Patients with Depression. American Family Physician. 2011;84(9):online-online. Accessed August 4, 2023. https://www.aafp.org/pubs/afp/issues/2011/1101/od1.html.
Thomas A, Grandner M, Nowakowski S, Nesom G, Corbitt C, Perlis ML. Where are the Behavioral Sleep Medicine Providers and Where are They Needed? A Geographic Assessment. Behav Sleep Med. 2016 Nov-Dec;14(6):687-98. doi: 10.1080/15402002.2016.1173551. Epub 2016 May 9. PMID: 27159249; PMCID: PMC5070478.
Forma F, Knight TG, Thorndike FP, Xiong X, Baik R, Velez FF, Maricich YA, Malone DC. Real-World Evaluation of Clinical Response and Long-Term Healthcare Resource Utilization Patterns Following Treatment with a Digital Therapeutic for Chronic Insomnia. Clinicoecon Outcomes Res. 2022 Aug 10;14:537-546. doi: 10.2147/CEOR.S368780. PMID: 35983014; PMCID: PMC9379126.
Espie CA, Kyle SD, Williams C, et al. A Randomized, Placebo-Controlled Trial of Online Cognitive Behavioral Therapy for Chronic Insomnia Disorder Delivered via an Automated Media-Rich Web Application. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3353040/.
Vincent N. Logging on for nodding off: Mendeley. 2018;32(6):123-126. Accessed August 4, 2023. https://www.mendeley.com/catalogue/330ca30f-5a53-3e0a-add8-c59804136a96/.
Ong JC, Shapiro SL, Manber R. Combining mindfulness meditation with cognitive-behavior therapy for insomnia: a treatment-development study. Behav Ther. 2008 Jun;39(2):171-82. doi: 10.1016/j.beth.2007.07.002. Epub 2007 Nov 14. PMID: 18502250; PMCID: PMC3052789.
Rusch HL, Rosario M, Levison LM, Olivera A, Livingston WS, Wu T, Gill JM. The effect of mindfulness meditation on sleep quality: a systematic review and meta-analysis of randomized controlled trials. Ann N Y Acad Sci. 2019 Jun;1445(1):5-16. doi: 10.1111/nyas.13996. Epub 2018 Dec 21. PMID: 30575050; PMCID: PMC6557693.
Grierson AB, Hobbs MJ, Mason EC. Self-guided online cognitive behavioural therapy for insomnia: A naturalistic evaluation in patients with potential psychiatric comorbidities. 2020;266:305-310. doi:https://doi.org/10.1016/j.jad.2020.01.143.
Internet-based cognitive behaviour therapy for insomnia before and during the COVID-19 pandemic. Australian Psychologist. Published 2022. Accessed August 4, 2023. https://www.tandfonline.com/doi/abs/10.1080/00050067.2021.1979884?journalCode=rapy20.
Jacobs GD, Pace-Schott EF, Stickgold R, Otto MW. Cognitive Behavior Therapy and Pharmacotherapy for Insomnia. 2004;164(17):1888-1888. doi:https://doi.org/10.1001/archinte.164.17.1888.
Walker J, Muench A, Perlis ML, Vargas I. Cognitive Behavioral Therapy for Insomnia (CBT-I): A Primer. Klin Spec Psihol. 2022;11(2):123-137. doi: 10.17759/cpse.2022110208. PMID: 36908717; PMCID: PMC10002474.
Godzik C, Crawford SL, Ryan EG. Feasibility of an online cognitive behavioral therapy program to improve insomnia, mood, and quality of life in bereaved adults ages 55 and older. https://www.sciencedirect.com/science/article/abs/pii/S0197457220303712.
Cognitive Behavioral Therapy for Insomnia (CBT-I) | Sleep Foundation. Sleep Foundation. Published September 15, 2020. Accessed July 30, 2023. https://www.sleepfoundation.org/insomnia/treatment/cognitive-behavioral-therapy-insomnia.
Rossman J. Cognitive-Behavioral Therapy for Insomnia: An Effective and Underutilized Treatment for Insomnia. Am J Lifestyle Med. 2019 Aug 12;13(6):544-547. doi: 10.1177/1559827619867677. PMID: 31662718; PMCID: PMC6796223.
Anderson KN, Goldsmith P, Gardiner A. A pilot evaluation of an online cognitive behavioral therapy for insomnia disorder – targeted screening and interactive Web design lead to improved sleep in a community population. Nat Sci Sleep. 2014 Mar 17;6:43-9. doi: 10.2147/NSS.S57852. PMID: 24669197; PMCID: PMC3962311.
Internet-Based Cognitive Behavioral Therapy for Insomnia in Appalachian Women: A Pilot Study. Behavioral Sleep Medicine. Published 2020. Accessed July 30, 2023. https://www.tandfonline.com/doi/full/10.1080/15402002.2019.1661249.
Bertisch S. Cognitive behavioral therapy for insomnia by telemedicine: Is it as good as in-person treatment? – Harvard Health. Harvard Health. Published June 15, 2021. Accessed July 30, 2023. https://www.health.harvard.edu/blog/cognitive-behavioral-therapy-for-insomnia-by-telemedicine-is-it-as-good-as-in-person-treatment-202106152488.
Thiart H, Ebert DD, Lehr D, Nobis S, Buntrock C, Berking M, Smit F, Riper H. Internet-Based Cognitive Behavioral Therapy for Insomnia: A Health Economic Evaluation. Sleep. 2016 Oct 1;39(10):1769-1778. doi: 10.5665/sleep.6152. PMID: 27450686; PMCID: PMC5020359.
Behavioral Treatments. Harvard.edu. Published 2023. Accessed July 30, 2023. https://sleep.hms.harvard.edu/education-training/public-education/sleep-and-health-education-program/sleep-health-education-64.
Junna, M. Think your way to sleep: Cognitive behavioral therapy for insomnia – Mayo Clinic Press. Mayo Clinic Press. Published October 19, 2022. Accessed July 30, 2023. https://mcpress.mayoclinic.org/living-well/think-your-way-to-sleep-cognitive-behavioral-therapy-for-insomnia/.




