“What I’m saying, in a nutshell, is that mitochondrial dysfunction is ultimately the cause of mental illness.” (Dr. Chris Palmer)
Table of Contents
This article may contain compensated links. Please read Disclaimer for more info. As an Amazon Associate, I earn from qualifying purchases.
Does the word “mitochondria” sound vaguely familiar?
Congratulations! Something has stuck with you from your ninth-grade biology class.
But what’s the buzz about mitochondria dysfunction lately? All that talk about mitochondrial health? Mitochondrial support? Mitochondria diet?
The list is long.
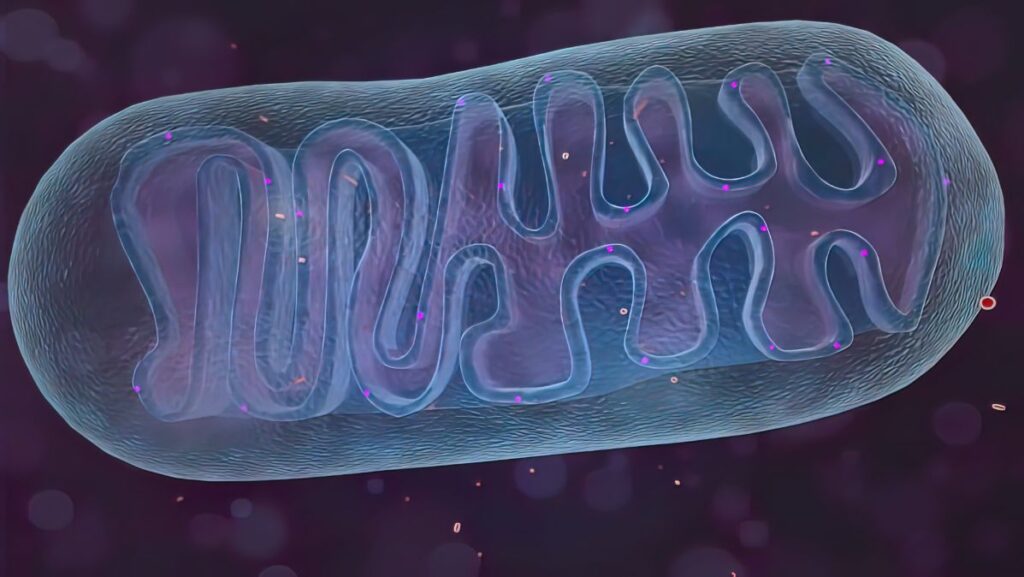
For sure, you’ll also remember that mitochondria were simplified as the “powerhouses” of the cell. Like little energy factories working non-stop to fuel physical processes of your body.
But again, what’s the relationship to mental health?
In the last couple of years, research into the relationship between metabolism, mitochondria, and mental health has exploded. Scientists are able to connect more and more dots.
And those new mitochondria facts might fascinate the pants off of you.
So, hang tight to learn more about how healthy mitochondria can help you with mental health struggles.
1 Beyond Neurotransmitters: Minding Your Mitochondria for Mental Health
When we think of mental health, we often focus on the workings of our brains and the connections between neurons. You know, dopamine, serotonin, and all the other neurotransmitters.
So, lots of antidepressants are prescribed to tackle that aspect of the brain: changing the neurotransmission levels in the brain.
However, these pills come with a truckload of side effects. And studies show that only a lucky 20% find real relief from antidepressants.
Unraveling the complex biology of psychiatric disease is like peeling back onion layers, with neurotransmitters, stress, genetics, trauma, and more adding to the mix.
But here’s the kicker: despite modern medicine’s advancements, many current treatments still leave us teary-eyed and craving better options.
That’s where the study of mitochondria and their relationship to mental health comes in.
Mitochondria might hold the key to understanding anxiety and depression. And a whole lot of other mental disorders, such as bipolar and schizophrenia.
Specialists like Dr. Chris Palmer, Professor of Psychiatry at Harvard Medical School, have been diving deep into researching the connection between mental health symptoms and problems with metabolism and mitochondria.
The core message?
Mental disorders are actually metabolic disorders of the brain. That means minding your mitochondria might improve your quality of life dramatically if you are suffering from depression, schizophrenia, anxiety, or other mental health disorders.
Sounds too enticing to be true?
Probably. But scientists are working hard to find out about this theory of neuron mitochondria, with numerous studies done to promote mental well-being.
It’s a revolutionary idea that could lead to more advanced and much safer treatment methods compared to what mainstream psychiatry uses today.

2 Metabolic Masters: Mitochondria Energy Production for the Brain
Human brains are energy-hungry machines—Neurons, the brain’s building blocks, demand more energy than many other cells in our body.
Despite the brain comprising just 2% of our body weight, around 20% of our oxygen and 25% of our glucose go directly to fueling the brain.
To meet this demand, neurons house a large number of mitochondria. These produce adenosine triphosphate (ATP), the cell’s primary energy currency, through a process called oxidative phosphorylation.
Consider this: dopamine-producing neurons, for instance, may require up to 1 million mitochondria. That’s quite a fleet!
So, maintaining a robust army of healthy mitochondria becomes critical for optimal brain function and mental well-being.
On the other hand, when mitochondrial capacity falters, energy production takes a hit. This can contribute to a range of brain-related issues, from extreme fatigue, cognitive decline, and mood problems to various psychiatric disorders.
3 When Stress Strikes: The Cell Danger Response
Mitochondria might spend their days as the “powerhouses of the cell” but clearly moonlight in an array of other activities.
Mitochondria are not simply the powerhouses of your cells. They actually have two crucial jobs:
Besides tirelessly generating energy for our cells to fuel all our activities, they also react to stressors. Once sensing danger, they release special molecules that serve as signals. This allows cells to communicate and protect themselves in times of trouble.
Enter Dr. Robert Naviaux and his groundbreaking concept: the Cell Danger Response (CDR).
During the CDR, mitochondria switch gears, shifting their focus from energy production to fortifying and fixing the cell.
This reaction is significant because it has the potential to disrupt cellular function, trigger chronic inflammation, and mess with your cells’ functioning.
And, yes, you’ve guessed it. This disruption has been linked to a host of mental health conditions.
So, it’s like our cells have this built-in defense mechanism, but when it goes haywire, it can wreak havoc on our mental well-being.

4 Connecting the Dots: Neuroplasticity, Mental Health, and Mitochondrial Dysfunction
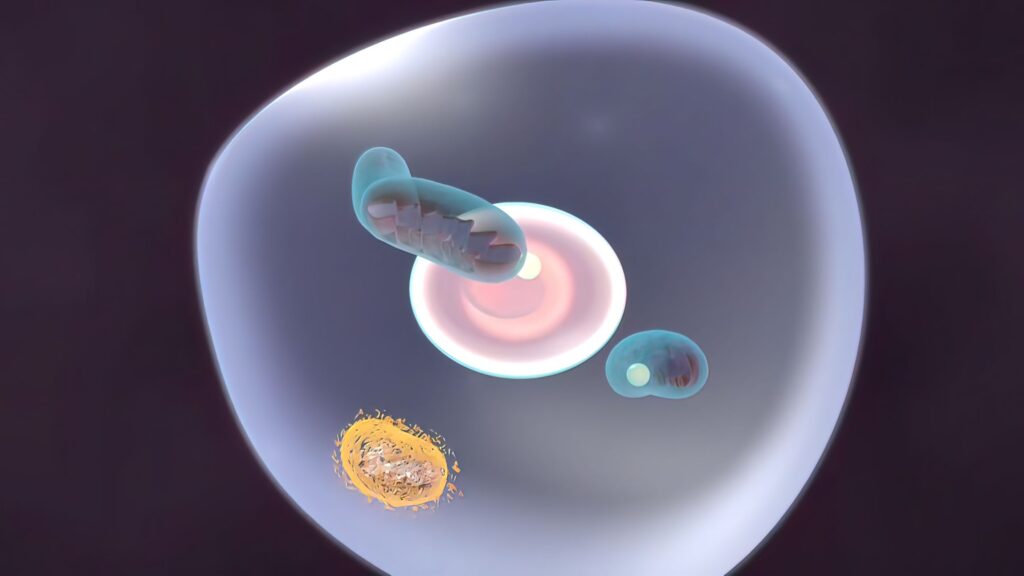
When mitochondria stop making energy their main priority, it can leave the central nervous system running low on energy.
The impact of this can show up in different ways, such as:
- It affects the production of neurotransmitters, the chemicals responsible for brain cell communication. This can throw mood, cognition, and behavior off balance.
- Low brain energy interferes with neurotrophic factors, the proteins that help nerve cells grow and survive. These factors are key to neuroplasticity—your brain’s ability to reshape itself in response to things happening around you. This way, your brain has a hard time handling stress, regulating moods, and processing trauma as it should.
- Rogue mitochondria in brain cells can ignite brain inflammation, again paving the way for mental health disorders.
The connection between wonky mitochondria and mental health seems astounding. At the same time, focusing on these misbehaving juggernauts could hold the key to unlocking a new era of mental well-being. So keep reading.
5 The Right Balance: Mitochondria’s Dual-Edged Sword of Functionality
When it comes to mito dysfunction, one word sums it up nicely: stress.
But wait, stress isn’t necessarily the villain. Both too much and too little stress can disrupt how your mitochondria produce energy.
Just like you, mitochondria thrive on some stress. It’s called hormesis—the perks of exercise or challenging tasks.
These “good” stresses trigger reactive oxygen species (ROS), boosting protective mechanisms.
ROS play a role in immune responses and cellular signaling, contributing to important processes such as cell growth, defense against pathogens, and regulation.
But here’s the twist: When stress overwhelms you, it takes a toll on your well-being, keeping mitochondria in defense mode. ROS levels exceed the body’s antioxidant defense mechanism, leading to chronic activation, uncontrolled growth, and inflammation.
Furthermore, your mitochondria can’t generate enough ATP to fuel your cells because they are preoccupied with the defense task.
These factors damage mitochondrial DNA (mtDNA), leading to aging and a plethora of health issues.

6 Mitochondria’s Foes: Battling Stressors for Optimal Health
So, what exactly are the stressors that disrupt the normal functioning of mitochondria? And how can you mind your mitochondria to feel better?
Biochemical, psychological, or behavioral factors can all contribute to stress.
Working too much, going crazy with exercise, dealing with inflammation, carrying extra weight, not getting the right nutrients, exposing yourself to toxins, and many other lifestyle factors can contribute to mitochondrial dysfunction.
Now, let’s dive into these stressors and see what they’re all about:
Poor Diet
According to the brain energy theory of mental illness, tweaking your diet can make a big difference in the lives of mental health sufferers.
Delicious breakfast toast and chocolate cake—all too tempting?
Well, here’s the problem.
When you eat a lot of high-calorie, low-nutrient foods, your mitochondria get overwhelmed with all that extra energy. This leads to inflammation and can trigger depression and other mental problems.
Who knew eating those cookies could have such evil consequences?
The link between simple carbohydrates and mood problems has been recognized for decades. Some psychiatrists recommend the ketogenic diet, swapping fats for carbs. It provides a stable brain energy source and improves mitochondrial efficiency.
An extra plus: low-carb diets may also positively impact the microbiome, which has been linked to conditions like anxiety, depression, Parkinson’s disease, and Alzheimer’s.
But remember, low-carb isn’t for everyone. Check with your doctor before making any drastic changes, especially if you’re pregnant, have eating disorders, hypothyroidism, or are a high-performance athlete.
And then there is intermittent fasting—an eating pattern that involves alternating periods of fasting and eating.
A Harvard study found that it activates a protein called AMPK, which promotes healthy aging and keeps our mitochondria in a youthful state. Mitochondria can become less connected as we age, but intermittent fasting helps maintain their organization and connectivity.
While intermittent fasting has astonishing benefits for your overall health and slows down aging, it’s also not suitable for everyone. Don’t do it if you have medical conditions like diabetes or a history of anorexia nervosa.
One thing everyone can do?
Ditch highly processed foods and go for natural whole foods. Your mitochondria will thank you for the nutrients they need to thrive.

Inappropriate Ways of Exercising
The right kind of exercise can do wonders for mitochondria. It can give them a turbo boost to keep you feeling energized and healthy.
But like any good thing, there’s a balance to be found. Both too much and too little exercise can throw your mitochondria off track.
When you overexercise, your mitochondria will become overwhelmed. They start churning out excessive reactive oxygen species (ROS) and trigger inflammation.
On the other hand, living a sedentary lifestyle is equivalent to denying the purpose of mitochondria. They miss out on that gentle nudge to keep them on their toes. Without activation, your mitochondria become sluggish and fail to perform at their best. We need to give them some action to trigger their protective mechanisms, improve insulin sensitivity, and maintain their quality control strategies.
Therefore, remember to find that sweet spot where you can challenge yourself without sending your mitochondria into a frenzy.

Bad Quality Sleep
Sleep plays a vital role in maintaining optimal brain health and function.
During sleep, the glymphatic system acts as a detoxification mechanism for the brain, clearing out neurotoxic waste and promoting overall brain well-being.
But here’s the thing: If you skimp on sleep or toss and turn all night, the glymphatic cleaning crew can’t do its job properly.
The result?
Harmful substances like amyloid beta start to build up, wreaking havoc on your mitochondrial health. And subsequently your brain health.
Dysfunctional mitochondria have been associated with cognitive decline, memory impairment, and mental health disorders. Research has even observed glymphatic system dysfunction surrounding the hippocampus and cortex in animal models of depression.
Prioritizing good sleep habits can have significant benefits for mental well-being and cognitive abilities.

Disruption of Circadian Rhythm
The circadian rhythm, your body’s internal clock, regulates vital processes like hormone production, digestion, body temperature, and overall physiology. It guides you when to sleep, wake up, and carry out these functions.
When natural light exposure is lacking or your circadian rhythm is disrupted, it can impair the mitochondria’s quality control process called mitophagy. This leads to mitochondrial degeneration.
One culprit for disrupting your circadian rhythm is staying up late, especially with excessive screen time emitting blue light.
This interferes with melatonin production, the hormone regulating your sleep-wake cycle, and other hormones.
Furthermore, neurotransmitters like Gaba, serotonin, and dopamine, vital for mood and brain function, are also influenced by your circadian rhythm. Inadequate light exposure and sleep deprivation can throw these neurotransmitters off balance, affecting your overall well-being.
So, it’s important to prioritize natural light exposure and maintain healthy sleep patterns to support the proper functioning of our mitochondria and promote optimal health.

Poor Gut Health
Did you know that your gut and mitochondria are in cahoots?
Mitochondria are essential for your gut cells to keep your digestive system in shape. They produce the energy needed to maintain cell junctions. But when they go haywire, you can end up with a leaky gut—that means your intestinal lining becomes permeable.
No good news.
Ongoing inflammation caused by a leaky gut makes the immune system go into overdrive. And there’s a growing body of evidence suggesting that this can mess with your mood and mental health.
But fear not.
You can support your gut, mitochondria, and mental well-being. Start by embracing a balanced diet, chock-full of probiotic-rich foods. And watch out for anything that might disrupt your gut microbiota.

Dysregulated Calcium Levels
Did you know that calcium and mitochondria have an intricate connection that affects our mental health?
Calcium is a key player in cellular signaling, while mitochondria act as the guardians of calcium balance within our cells. They act as regulators, managing the levels of calcium by taking it in or releasing it as needed.
Maintaining this delicate balance is crucial for the optimal functioning of mitochondria. Too much or too little calcium can throw them off track and lead to dysfunction.
Now, here’s where it gets interesting.
When calcium homeostasis goes haywire, it can have a profound impact on our mental well-being.
Excessive calcium influx into our neuronal cells, known as excitotoxicity, can wreak havoc on our brain circuits. This process is implicated in various mental health issues, like mood disorders, schizophrenia, and neurodegenerative diseases.
But that’s not all.
Calcium signaling is closely linked to neurotransmitter release and synaptic plasticity, which are essential for cognitive function and mood regulation.
In mitochondria, calcium signaling can disrupt synaptic plasticity and neurotransmitter release. This potentially leads to mood disorders and cognitive disabilities.
Researchers are delving into the mechanisms behind calcium dysregulation and its impact on mitochondrial function. Their aim? Creating treatments that fix the calcium imbalance, protect mitochondrial health, and alleviate symptoms of psychiatric illnesses.

Toxicity
Mitochondria are very susceptible to the harmful effects of various toxins in our environment. Here are some culprits that can throw them off balance:
- Pharmaceuticals: Certain medications like statins and antibiotics can mess with mitochondrial function. Statins, the popular cholesterol-lowering drugs, have been linked to mitochondrial damage. And antibiotics such as quinolones and aminoglycosides can disrupt mitochondrial health due to our shared bacterial heritage.
- Pesticides and herbicides: These chemicals meant to battle pests and weeds can harm mitochondria too. Since mitochondria have ancestral ties to bacteria, they can fall victim to the toxic effects of these substances.
- Moulds: Mycotoxins produced by moulds are no friends of mitochondria. They can unleash oxidative damage and trigger a programmed cell death party within these energy factories.
- Infections: Viruses and bacteria can be both allies and foes for our mitochondria. While mitochondria release reactive oxygen species (ROS) to combat bacterial invaders, they can also be compromised by certain strains of bacteria.
- Metals: Toxic metals like mercury, cadmium, lead, aluminium, easily lead to dysfunctional mitochondria. They interfere with the normal workings of mitochondria, contributing to mental health problems.
- Hydrocarbons: Lighting up a cigarette? Beware of the hydrocarbons in smoke. They increase oxidative stress and put a strain on mitochondrial function.
- Radiation: Turns out, radiation isn’t a friend to mitochondria either. Studies have shown that exposure to radiation can damage these cellular powerhouses, hindering their energy production abilities.
- Endogenous metabolites: In neurodegenerative diseases like Parkinson’s and Alzheimer’s, misfolded proteins and metabolites from neurotransmitters can turn against mitochondria, causing further disruption.
To keep your mitochondria in good shape, it’s important to be cautious of toxins. Be mindful of the medications you use, reduce exposure to harmful chemicals, and create a healthy environment. These steps can greatly contribute to preserving the health of your mitochondria.

Psychological Trauma
Psychological trauma packs a punch on your mitochondria and affects your overall well-being. Here are some of the key impacts:
- Hormone and neurotransmitter imbalances: Stress sends hormones and neurotransmitters on a rollercoaster ride. When cortisol and adrenaline surge due to chronic or intense stress, they burden mitochondria with excessive glucose and lipids.
- Increased production of ROS: Long-term psychological stress revs up reactive oxygen species (ROS) production in mitochondria. This disrupts oxidative phosphorylation, cranks up oxidative stress, and endangers mitochondrial DNA and function.
- Insulin resistance: Chronic stress fuels glucose spikes, raising the risk of insulin resistance. As cells struggle to handle insulin and glucose, mitochondrial function takes a hit.
- Thyroid hormone disruption: Stress equally messes with thyroid hormones, especially T3 and T2, crucial for mitochondrial mojo. These hormones power up oxidative phosphorylation and mitochondrial biogenesis.
And that’s not all. Psychological stress can cause mitochondrial DNA to leak into the bloodstream. Mitochondrial components—DAMPs—trigger an immune response, lighting the inflammation fuse.

Aging
As the years pass, you experience a decline in mitochondrial performance. Mutations in mitochondrial DNA (mtDNA) and dwindling ATP production are to blame.
Research suggests that a drop in ATP exceeding 20% with age may fuel neurological diseases.
But here’s the silver lining: Exercise plays a key role in maintaining mitochondria. It can stimulate mechanisms that help repair mutated mtDNA and promote the growth of fresh mitochondria, a process known as mitochondrial biogenesis.
So, as you gracefully age, lace up those sneakers and embrace regular exercise. It revs up your neurons, shields you against neurological woes, and nurtures your mitochondria’s vitality.

7 Targeted Mitochondria Support: Navigating Medications and Supplements Wisely
According to Dr. Chris Palmer, lifestyle changes like sleep, diet, and exercise should take center stage when you want to reclaim mitochondrial health. However, it’s important to understand how additional interventions can benefit (or harm) you.
Prescription meds, especially psychiatric drugs, often disrupt mitochondrial function and metabolism, leading to ATP disorder with weight gain, type 2 diabetes, and other health issues. Therefore, it would be ideal to take as little of those meds as possible.
But careful! Don’t quit your pills abruptly since that can get dangerous. Work with a healthcare provider to find out if and how to safely transition away from them and regain control over your mitochondrial health.
As for supplements, researchers have been exploring their potential benefits for decades, seeking ways to counter mitochondrial dysfunction and oxidative stress. Antioxidants like vitamin E and C seemed like the silver bullet, but taking antioxidant pills alone isn’t the answer. The story is more complicated.
Finding the right balance and timing is key.
Supplements should neither be overdone nor underdone. If you have nutrient deficiencies, temporary supplementation can help replenish your stores. But remember, it’s crucial to identify the root causes of these deficiencies and address them (looking at you, diet).
While specific supplements like omega-3, B vitamins, iron, magnesium threonate, and more show promise in boosting mitochondrial efficiency, research is still at the tip of the iceberg. More studies are needed to uncover their full potential.
Read more about possible supplements here.

Embracing the Journey: Mitochondrial Healing for Mental Well-Being
The journey into understanding the intricate relationship between mitochondrial health and mental well-being reveals a promising path forward.
While traditional therapies have their merits, they often miss the mark when it comes to addressing the underlying issues.
It’s time to shift our focus to the functioning of metabolism and unlock the true potential of mitochondria. By taking a holistic approach and nurturing your metabolic machinery, you can enhance the effectiveness of current treatments and embark on a new era of healing.
This exciting frontier offers personalized interventions that can revolutionize the lives of those battling mood disorders.
Your body possesses remarkable healing abilities; you just need to provide it with the opportunity to thrive.

Key Points and FAQ
How do mitochondria function?
Mitochondria function by using a process called oxidative phosphorylation to generate ATP, the energy molecule. They take in nutrients, such as carbohydrates and fats, and through a series of chemical reactions, extract energy from them. This energy is then used to fuel various cellular activities, ensuring the proper functioning of the body.
What are mitochondrial dysfunction symptoms?
Mitochondrial dysfunction can present with a wide range of symptoms that vary from person to person. Common symptoms include fatigue, muscle weakness, exercise intolerance, neurological problems (such as seizures and developmental delays), gastrointestinal issues, vision and hearing problems, and increased susceptibility to infections. However, it’s important to note that mitochondrial dysfunction can manifest differently in different individuals.
What is mitochondrial dysfunction treatment?
The treatment of mitochondrial dysfunction focuses on managing symptoms, optimizing mitochondrial function, and addressing underlying causes if possible. Treatment may involve a multidisciplinary approach, including medications to alleviate specific symptoms, supplements to support mitochondrial function, lifestyle modifications to promote overall health and management of associated medical conditions.
What is the general mitochondrial dysfunction definition?
Mitochondrial dysfunction refers to a condition where the mitochondria, which are the energy-producing structures within our cells, are not functioning properly. This can lead to a decrease in the production of ATP, the energy currency of the cell, and can affect various organs and systems in the body.
The energy deficit can lead to a wide range of symptoms, including fatigue, muscle weakness, exercise intolerance, and cognitive impairment.
Moreover, mitochondria are involved in various cellular processes beyond energy production, such as calcium regulation, reactive oxygen species (ROS) management, and apoptosis (programmed cell death). When mitochondria malfunction, these processes can be disrupted, leading to cellular dysfunction and potential damage.
Additionally, mitochondrial dysfunction has been linked to a variety of health conditions, including neurodegenerative diseases, cardiovascular disorders, metabolic disorders, and psychiatric disorders.
What’s the link between mitochondrial dysfunction and psychiatric disorders?
Emerging research suggests a connection between mitochondrial dysfunction and psychiatric disorders. Mitochondrial abnormalities can affect the brain’s energy supply and lead to impaired neuronal function, potentially contributing to mental health conditions such as depression and bipolar disorder. While more studies are needed, understanding this link may help develop targeted treatments for these disorders.
What scientists are doing research in the field of mitochondria health and mental health?
Numerous scientists and researchers are exploring the relationship between mitochondrial health and mental health. They are investigating how mitochondrial dysfunction may contribute to psychiatric disorders, exploring potential biomarkers, and studying the effects of interventions targeting mitochondrial function.
Some notable researchers in this field include Dr. Douglas Wallace (Director of the Center for Mitochondrial and Epigenomic Medicine at Children’s Hospital of Philadelphia), Dr. Keshav Singh (National Sun Yat-sen University, Taiwan), Dr. Russell Swerdlow (University of Kansas School of Medicine), Prof. Michael Berk (Institute for Mental and Physical Health and Clinical Translation (IMPACT) at Deakin University), and Dr. Richard J. Youle (National Institute of Neurological Disorders) among others.
Stress and mitochondria, how are they related?
Chronic stress can disrupt mitochondrial activity, leading to increased production of reactive oxygen species and oxidative stress, which can further damage mitochondria.
Conversely, maintaining good mitochondrial health through lifestyle practices like stress reduction techniques, exercise, and adequate sleep can help mitigate the negative effects of stress on mitochondria.
What are mitochondrial disorders in the nervous system?
Mitochondrial disorders in the nervous system refer to conditions where mitochondrial dysfunction primarily affects the cells and tissues of the central nervous system (brain and spinal cord) or peripheral nervous system.
These disorders can manifest as a range of neurological symptoms, such as seizures, muscle weakness, developmental delays, movement disorders, and cognitive impairments, depending on the specific type and extent of mitochondrial dysfunction.
Can mitochondrial disease kill you?
Mitochondrial dysfunctions vary in severity. Only in some cases can mitochondrial disease be fatal. The impact on a person’s health depends on the specific type and extent of mitochondrial dysfunction.
How do you restore mitochondrial disorder?
Restoring mitochondrial disorder is a complex process that requires comprehensive medical management. Treatment options may include medications and supplements that target specific mitochondrial dysfunction, lifestyle modifications to support mitochondrial health, and managing underlying conditions associated with mitochondrial disease.
Is there a direct link between mitochondria and brain health?
Yes, there is a direct link between mitochondria and brain health. The brain requires a substantial amount of energy to function properly, and mitochondria play a crucial role in providing that energy. Healthy mitochondrial function is vital for maintaining the energy supply to brain cells, supporting optimal brain function, and overall cognitive health.
How do mitochondria affect mental health?
Mitochondria have a significant impact on mental health because they are responsible for generating energy that fuels the brain and supports proper neuronal function. When mitochondrial function is compromised, it can lead to decreased energy production, increased oxidative stress, and impaired brain cell communication, potentially contributing to mental health conditions such as anxiety, depression, and cognitive disorders.
How are mitochondrial disease and depression related?
Research suggests a possible link between mitochondrial dysfunction and depression. Mitochondrial abnormalities can disrupt the energy production process in brain cells, affecting neurotransmitter function and overall brain health.
What’s the link between bipolar and mitochondria?
There is ongoing research exploring the connection between bipolar disorder and mitochondrial dysfunction. Mitochondria play a role in energy production, and alterations in mitochondrial function can potentially impact brain function and contribute to the development or progression of bipolar disorder.
How do I improve mitochondrial health, and how can I repair my mitochondria naturally?
There are several lifestyle approaches that may support mitochondrial health naturally. These include maintaining a balanced and nutrient-rich diet, engaging in regular physical exercise, managing stress levels, getting sufficient sleep, and avoiding exposure to toxins. These practices can help optimize mitochondrial function and support overall cellular health.
What foods support mitochondria?
Certain foods are known to support mitochondrial health. These include nutrient-dense options like leafy green vegetables, berries, fatty fish rich in omega-3 fatty acids, nuts and seeds, whole grains, and legumes. These foods provide antioxidants, essential vitamins, minerals, and healthy fats that can help maintain mitochondrial function and support overall cellular health.
Energy, mitochondria, metabolism. How is it all related?
Mitochondria play a fundamental role in cellular energy production through a process called cellular respiration. They convert nutrients from the food we eat into ATP, which serves as the energy currency for all cellular functions. Proper mitochondrial function is essential for efficient metabolism and maintaining overall energy levels throughout the body.
What are mitochondrial dysfunction supplements?
Mitochondrial dysfunction supplements are dietary supplements that aim to support mitochondrial health and function. These may include antioxidants like coenzyme Q10 (CoQ10), alpha-lipoic acid, and vitamins C and E, as well as compounds like acetyl-L-carnitine and creatine, which are involved in cellular energy production. It’s important to consult with a healthcare professional before starting any new supplements.
What is the relationship between mitochondrial dysfunction and oxidative stress?
Mitochondrial dysfunction can contribute to increased oxidative stress within cells. When mitochondria are not functioning optimally, they produce higher levels of reactive oxygen species (ROS), which are harmful byproducts. Excessive ROS can lead to cellular damage and contribute to various health conditions. Managing mitochondrial dysfunction and reducing oxidative stress can be important for overall cellular health and well-being.
Is there a mitochondrial dysfunction test?
Yes, there are various tests available to assess mitochondrial dysfunction. These tests may involve analyzing biochemical markers in the blood, examining mitochondrial DNA, assessing cellular respiration rates, or conducting muscle biopsies. A healthcare professional experienced in mitochondrial disorders can recommend and interpret the most appropriate tests based on a person’s specific symptoms and medical history.
What is mitochondrial dysfunction in neurodegenerative diseases?
Mitochondrial dysfunction is believed to play a role in the development and progression of several neurodegenerative diseases, including Parkinson’s disease, Alzheimer’s disease, and Huntington’s disease. Impaired mitochondrial function can lead to energy deficits, increased oxidative stress, and impaired protein handling, contributing to the degeneration of neurons and the progression of these diseases.
What is the relationship between mitochondrial dysfunction and aging?
As we age, the function and efficiency of mitochondria decline, leading to reduced energy production and increased production of reactive oxygen species (ROS). This mitochondrial dysfunction and increased oxidative stress contribute to cellular damage, tissue degeneration, and age-related diseases, ultimately impacting overall health and accelerating the aging process.

Sources
Adams, J. U. (2008). Human Evolutionary Tree. Nature Education, 1(1), 145
https://www.nature.com/scitable/topicpage/Human-Evolutionary-Tree-417
Alzheimer’s Association. (2021). 2021 Alzheimer’s disease facts and figures. Alzheimer’s & Dementia, 17(3), 327–406. https://doi.org/10.1002/alz.12328
Bélanger, M., Allaman, I. et al. (2011). Brain energy metabolism: focus on astrocyte-neuron metabolic cooperation. Cell Metabolism, 14(6), 724–738.
Biskup, S. et al. (2006). Detrimental deletions: Mitochondria, aging and Parkinson’s disease. Bioessays, 28(10), 963–967. https://doi.org/10.1002/bies.20471
Boesch, P. et al. (2011). DNA repair in organelles: Pathways, organization, regulation, relevance in disease and aging. Biochimica et Biophysica Acta—Molecular Cell Research, 1813(1), 186–200. https://doi.org/10.1016/j.bbamcr.2010.10.002
Bratic, A., & Larsson, N.-G. (2013, March 1). The role of mitochondria in aging. The Journal of Clinical Investigation, 123(3), 951–957
https://www.jci.org/articles/view/64125
Cao, X. et al. (2012). Effects of exercise intensity on copy number and mutations of mitochondrial DNA in gastrocnemus muscles in mice. Molecular Medicine Reports, 6, 426–428. https://doi.org/10.3892/mmr.2012.913
Cenini, G. et al. (2019). Mitochondria as potential targets in Alzheimer disease therapy: An update. Frontiers in Pharmacology, 10, Article 902. https://doi.org/10.3389/fphar.2019.00902
Chan, D. C. (2006, June 30). Mitochondria: Dynamic organelles in disease, aging, and development. Cell, 125(7), 1241–1252
https://www.sciencedirect.com/science/article/pii/S0092867406007689
Chan, D. C. (2012). Fusion and fission: Interlinked processes critical for mitochondrial health. Annual Review of Genetics, 46, 265–287. https://doi.org/10.1146/annurev-genet-110410-132529
Chial, H., & Craig, J. (2008). mtDNA and mitochondrial diseases. Nature Education, 1(1), 217
https://www.nature.com/scitable/topicpage/mtdna-and-mitochondrial-diseases-903
Deheshi, S. et al. (2013). Mitochondrial trafficking in neuropsychiatric diseases. Neurobiology of Disease, 51, 66–71. https://doi.org/10.1016/j.nbd.2012.06.015
DiMauro, S., & Davidzon, G. (2005). Mitochondrial DNA and disease. Annals of Medicine, 37(3), 222–232
http://www.med.unc.edu/neurology/files/documents/child-teaching-pdf/Mitochondrial%20Review%20DiMaro%2005.pdf
Frye, R. E. et al. (2011). Mitochondrial dysfunction can connect the diverse medical symptoms associated with autism spectrum disorders. Pediatric Research, 69(8), 41–47. https://doi.org/10.1111/j.1469-8749.2011.03980.x
Gardner, A. (2011). Beyond the serotonin hypothesis: Mitochondria, inflammation and neurodegeneration in major depression and affective spectrum disorders. Progress in Neuro-Psychopharmacology and Biological Psychiatry, 35(3), 730–743. https://doi.org/10.1016/j.pnpbp.2010.07.030
Geary, D. C. (2019). The spark of life and the unification of intelligence, health, and aging. Current Directions in Psychological Science, 28(3), 223–228. https://doi.org/10.1177/0963721412469398
Green, D. R. et al. (1998). Mitochondria and apoptosis. Science, 1309–1312. https://doi.org/ 10.1126/science.281.5381.1309
Grimm, A. et al. (2017). Brain aging and neurodegeneration: From a mitochondrial point of view. Journal of Neurochemistry, 143(4), 418–431. https://doi.org/10.1111/jnc.14037
Huang, Y. et al. (2012). Effects of age and amyloid deposition on Aß dynamics in the human central nervous system. Archives of Neurology, 69, 51–58. https://doi.org/10.1001/archneurol.2011.235
Kaplan, B. J. (2015). The emerging field of nutritional mental health: Inflammation, the microbiome, oxidative stress, and mitochondrial function. Clinical Psychological Science, 3(6), 964–980. https://doi.org/10.1177/2167702614555413
Klinge, C. M. (2008, December 15). Estrogenic control of mitochondrial function and biogenesis. Journal of Cellular Biochemistry, 105(6), 1342–1351
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2593138/
Kramer, P. et al. (2018). Our (mother’s) mitochondria and our mind. Perspectives on Psychological Science, 13(1), 88–100. https://doi.org/10.1177/1745691617718356
Mishra, P., & Chan, D. C. (2014, October). Mitochondrial dynamics and inheritance during cell division, development and disease. Nature Reviews Molecular Cell Biology, 15(10), 634–646
https://www.ncbi.nlm.nih.gov/pubmed/25237825
Mitochondrion — much more than an energy converter. (n.d.)
http://bscb.org/learning-resources/softcell-e-learning/mitochondrion-much-more-than-an-energy-converter/
Niccoli, T. et al. (2012). Ageing as a risk factor for disease. Current Biology, 22(17), R741–R752. https://doi.org/10.1016/j.cub.2012.07.024
Oliveira, G. et al. (2005). Mitochondrial dysfunction in autism spectrum disorders: A population-based study. Developmental Medicine and Child Neurology, 47(3), 185–189
https://www.ncbi.nlm.nih.gov/pubmed/15739723
Pagliarini, D. J. et al. (2013). Hallmarks of a new era in mitochondrial biochemistry. Genes & Development, 27(24), 2615–2627. https://doi.org/10.1101/gad.229724.113
Picard, M. et al. (2014). Mitochondria impact brain function and cognition. Proceedings of the National Academy of Sciences, 111(1), 7-8. https://doi.org/10.1073/pnas.1321881111
Rango, M. et al. (2018). Brain mitochondria, aging, and Parkinson’s disease. Genes, 9(5), 250. https://doi.org/10.3390/genes9050250
Rossier, M. F. (2006, August). T channels and steroid biosynthesis: In search of a link with mitochondria. Cell Calcium, 40(2), 155–164
https://www.sciencedirect.com/science/article/pii/S0143416006000856
Taylor, S. W. et al. (2003). Characterization of the human heart mitochondrial proteome. Nature Biotechnology, 21(3), 281–286
https://www.ncbi.nlm.nih.gov/pubmed/12592411
Wang, C. et al. (2009, February 22). The role of mitochondria in apoptosis. Annual Review of Genetics, 43, 95–118
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4762029/
What is mitochondrial disease? (n.d.)
https://www.umdf.org/what-is-mitochondrial-disease/
Youle, R. J. et al. (2012). Mitochondrial fission, fusion, and stress. Science, 337(6098), 1062–1065. https://doi.org/10.1126/science.1219855




